Winter’s high levels of respiratory syncytial virus (RSV) infections have come early this year and appear to be infecting more babies and small children and making them sicker than usual. This is contributing to the extreme pressure on many GPs and paediatric hospitals.
At the end of October, Children’s Health Ireland (CHI) reported a 50 per cent increase in the number of children attending their Emergency Departments (EDs) in Temple Street, Crumlin and Tallaght and the Urgent Care Unit in Blanchardstown, compared to the same period in 2019, which was their busiest year on record..
RSV causes about 80 per cent of the illness known as bronchiolitis (inflammation of the small airways in the lung). Currently about 40 per cent of babies/children being diagnosed with bronchiolitis at CHI centres are being admitted, compared with an admission rate of 30 per cent last year, reports Dr Carol Blackburn, consultant in paediatric emergency medicine at CHI Crumlin.
Why they seem to be sicker, “we’re not sure”, she says, “but it is obviously very concerning, because the smaller you are, the sicker you will be with this and the more help you are likely to need. Therefore, the more likely it is you will need a couple of nights in hospital to help you out.”
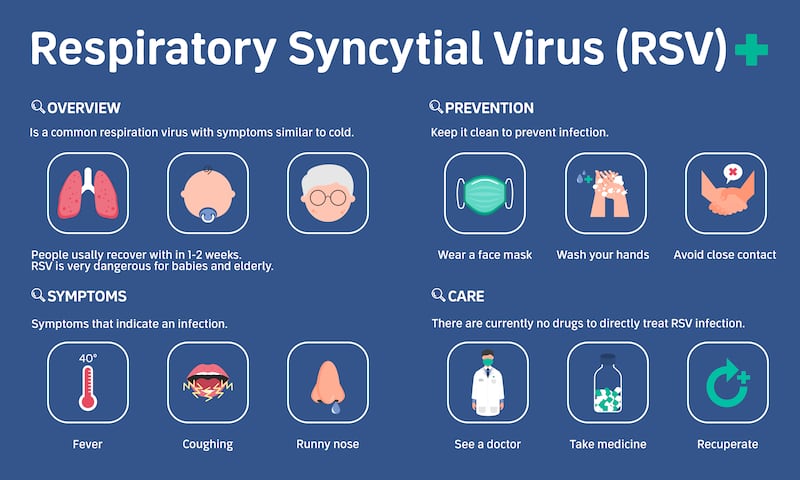
What is RSV?
It stands for Respiratory Syncytial Virus, a very common and very contagious virus that causes cold-like symptoms initially but can lead to worrying complications in a small minority of cases. Nearly all children will have had at least one infection of RSV by the age of two and for most it will cause a mild cold. However, it can develop into bronchiolitis or pneumonia.
In temperate climates such as ours, RSV epidemics typically occur from October to April, peaking in December/January. It has been a notifiable infectious disease in Ireland since January 2012. The Health Protection Surveillance Centre, which collects data from designated GP practices and hospitals to analyse trends on a weekly basis, was reporting “very high levels” by mid-November. Some 65 per cent of notified RSV cases were in those aged four and under. The current weekly increases in cases are expected to continue at least into next month, if not January
Despite the ubiquity of RSV, a recent survey found a relatively low level of public awareness and understanding of the virus. Just over half (53 per cent) of Irish parents had heard of RSV, according to research commissioned by Sanofi, and only one in five indicated knowing much about it.
What are the symptoms?
Initially common ones, typical of any upper tract respiratory illness, are a snotty nose, a slightly raised temperature and maybe a dry cough. “Snuffly symptoms” is how Dr Máire Finn, a GP at Ennis Centric Health in Co Clare sums them up. “A percentage of the children will have simply that and nothing more.” But for babies that might mean poor feeding and fussiness. Signs that the infection is spreading to the lungs include a continued raised temperature, coughing, wheezing and what Blackburn describes as “increased work of breathing”. In babies that will peak at day three to four, she says, when they may have trouble feeding and may need to go on to oxygen.
How do I care for a child with RSV at home?
The mild symptoms are easy to manage, says Dr Finn, who is a spokeswoman for the Sanofi Together Against RSV Campaign, which aims to create greater awareness around the symptoms. As RSV is most dangerous among babies under a year, she advises parents of this age group to be on the lookout for their child being off their feeds. A raised temperature can be managed with paracetamol or ibuprofen if necessary, although, as the HSE advises, don’t give paracetamol to babies younger than two months old, or who weigh less than 7kg, unless it is prescribed by a doctor.
Dr Finn often recommends a bath, as the steam is good for decongesting a snotty nose, which can be very debilitating for a small child. “They don’t feed well if their nose is blocked,” she says. You do need to be vigilant that the child is not becoming dehydrated and infection is not spreading to the lungs.
When should I seek medical attention?
There are a couple of markers of RSV infection moving to the lungs that will show in the child’s breathing. “If a child is struggling, a small baby in particularly, they flare their nostrils,” says Finn. They also “belly-breathe” – instead of the belly comfortably rising and falling, the muscles in between the ribs are sucked in because the child is having to make a bigger effort to get oxygen in. “If the belly is sucked in and breathing quickly, then the child is distressed.”
A good rule of thumb, she suggests, is that any baby under three months, who has anything more than a snuffly nose, should be checked by a GP
These are danger signs, along with dehydration and exhaustion. A temperature that keeps spiking and can’t be brought under control with paracetamol or ibuprofen over 24 hours will make a child unwell. A dry nappy for more than six hours is a sign the child is not getting enough fluids and running into a bit of trouble. It could just be tiredness or the snuffling that is causing poor feeding, says Finn, but it would be an indication that they should see a doctor.
A good rule of thumb, she suggests, is that any baby under three months, who has anything more than a snuffly nose, should be checked by a GP. To parents of older babies and children, she says: “If you are concerned about your child, come to general practice. We will only refer into hospital if we are concerned – it is not something we do lightly.”
RSV can be fatal, but very rarely. Those cases are usually when the infection has progressed to the spongy part of the lungs, explains Dr Finn, resulting in pneumonia. “Those complications are more common in the vulnerable children.”
Dr Blackburn says managing the condition revolves around monitoring a baby’s feeding. “We advise parents who feel their baby is having difficulty finishing a feed, whether that is breastmilk or formula, to offer them smaller feeds more often. That way you are mitigating extra work they have to do to feed. If the baby is not managing at least half of their normal intake, then seek medical attention.”
While acknowledging there are “extreme limitations on access to primary care at the moment”, Dr Blackburn encourages parents to try that first, rather than going straight to an ED. But if you can’t get your child to a GP and you are worried, “we are here”, 24/7, she says. However, there is overcrowding, with potential risk of overcrowding for infants, and “because we are having a surge and because it is affecting small babies, our wait times are not what we would like them to be”.
Babies and children are seen in ED in accordance with the sickest first, so those in need of assessment, rather than requiring immediate intervention, such as oxygen and intravenous fluids, face wait times in excess of five hours at CHI centres, she warns, depending on the time of day.
Can doctors give medication to treat RSV?
No, because it is a virus. Dr Finn believes that one benefit of the Covid pandemic was that it raised public awareness of how viral infections are treated “supportively” and not with antibiotics. However, a child with a prolonged viral infection can get a secondary bacterial infection, in which case they will need antibiotics, but that is relatively unusual.
If your baby needs hospital admission for RSV, the “supportive care”, says Dr Blackburn, involves oxygen and/or feeding. A baby unable to feed will be given either a nasal gastric tube to feed or intravenous fluids. Babies who need more than standard oxygen aid will get a form of ventilatory support – high-flow nasal cannulas – or, in extreme cases, be admitted to intensive care. “But thankfully, those having to go to ICU at the moment is regular; we are not overwhelmed by that so far.”
What children are more likely to become sicker with RSV?
“If you’re under one, you are a sitting duck for this illness every winter,” says Dr Blackburn. The most vulnerable include those under six months old, those with another underlying condition, or with a heart problem. Premature babies are also at greater risk.
Mandy Daly of the Irish Neonatal Health Alliance, which is supporting the awareness campaign, points out that preterm infants are more vulnerable and susceptible to infections. “For some infants, an RSV infection can lead to serious complications and can even become life-threatening if the infection reaches the lower respiratory tract.”
Dr Finn says that a home where there is a smoker is also a risk factor for RSV complications in babies or children. “They are more likely to deteriorate quickly if they are in a smoky environment.”
Is there anything we can do to prevent RSV infections?
If you are a parent of a baby under three months, or one born prematurely, you should be trying to protect them from exposure to viruses at the moment, says Dr Blackburn. “It means limiting visitors, limiting outings to crowded spaces; careful hand-washing; coughing/sneezing etiquette and trying to keep older siblings who might have colds further away while they are symptomatic.”
Once one child has RSV, it is “virtually impossible” to stop it spreading within the home, says Dr Finn. But if you have a newborn, do try to keep them separate from an older child, she advises, or at least try to prevent kissing and other close interactions.
Hand hygiene was drilled into children and adults alike during the pandemic and it is an important precaution. But there is a balance between that and over-zealous disinfecting.
“There is a hygiene hypothesis about illness and children,” observes Dr Finn. “Too much protecting them doesn’t necessarily do them good long-term.” The immunity they build up through exposure to viruses is important, and less of that during the Covid pandemic, when children were isolated and distanced from others, is probably one of the reasons for this current high level of RSV.
There is a cohort of toddlers and small children who were not exposed to RSV in their first year or two of life because of isolation during Covid, says Dr Blackburn, and they are probably picking it up now. “While they are older and it’s not making them terribly sick, they are giving it to their infant siblings and it is making them sicker.”
If the symptoms are mild, can they go back to creche?
This is a real dilemma, acknowledges Dr Finn because, separate from medical considerations, RSV is a burden on families, in that children have to stay away from creche or school. If you have a number of children getting RSV in turn at least once during the winter, it can seem never-ending. But if a child goes back to the creche feeling well but still within a week of first symptoms, they could be spreading it.
“There is a public-health responsibility with every illness and there is personal responsibility but then how do you manage yourself and your family in practical terms?” says Dr Finn. Some creches insist a child should be seen by a GP, which is not helpful for over-stretched practices and can make a parent feel negligent if they don’t go.
“If the parent has the luxury of being able to keep the child at home and can stay at home with the child, that is the far better situation for all involved,” she adds.
Are you saying that my child could get RSV more than once this winter?
GPs do see children coming back again and again with RSV, but “the first presentation is often the worst”, says Dr Finn. Children seem to cope better with subsequent infections because they have built up some immunity. As recurrent infections are common, don’t start worrying that there must be underlying chest problems.
Could I get my child vaccinated against it?
There is no vaccine available yet for RSV, but very vulnerable babies can be given a monthly immunoglobulin injection in the winter season, which is administered through specialised services in hospitals. “But it is not available or necessarily helpful for children who are otherwise well,” says Dr Blackburn.
However, she appeals to every parent of a child aged two or over to avail of the flu vaccine for them. This is given as a spray in each nostril and takes about two weeks to work.
“At the moment we are not seeing much influenza but we are expecting it,” she adds. “If we have a big surge of influenza at a time when RSV is still surging, our services will be extremely challenged.”
Case study: My four-month-old in A&E
Sinéad Hingston-Green had never heard of RSV until she was sitting in the emergency department of a hospital with her four-month-old son Alby during a family trip to South Africa last April.
She was shocked how fast he had deteriorated, a week into their return to the native country of her husband, Michael Green, to celebrate his 40th birthday. After taking swabs and taking an X-ray, staff at the Pretoria hospital told her Alby had RSV, which had developed into bronchiolitis. He was admitted and stayed there on oxygen for a week.

“It was a very scary experience,” says Sinéad, who was in hospital alone with him while Michael looked after their other two children, Lily Hingston (10) and Dylan Green (four). Sinead’s first husband, Geoff Hingston, died tragically at the age of 37 while swimming on holidays in Portugal in the summer of 2011, when she was 19 weeks pregnant with Lily.
Seeing Alby become so sick evoked in Sinead some of the horror of that death. “There was that very real fear of ‘something could go wrong here’. I never in a million years thought anything would ever happen to Geoff that day and he died so suddenly. I guess when Alby got so sick, it was the trigger of that, but thank God he was absolutely fine.”
‘They had him on oxygen within 20 minutes of us arriving in A&E. His saturation levels were very low and he was really struggling to breathe’
Afterwards, there was parental guilt about whether he would have ended up on oxygen for a week if they had brought him to hospital sooner. “But he probably would have anyway, because RSV attacks that quickly, especially because he was so small.” However, she reckons had they known the warning signs better, they would have acted faster. “Because I didn’t even know what RSV was – babies get snuffles all the time, I presumed it was that.”
During their first week in South Africa, the family stayed with Michael’s friends, whose young son had “a bit of a cough but nothing alarming”. But by end of the first weekend, Alby started to look unwell.
“He didn’t have a temperature or cough. His eyes were just kind of watery and red.” Within 24 hours, his nose became runny and a dry cough started. A couple of Michael’s medical friends advised them to keep an eye on it and gave them a hand-held nebuliser.
On the Tuesday they took Alby to a doctor to see if it was okay to go ahead with a planned trip to a private game reserve. “She said it hadn’t turned into anything yet, but that wasn’t to say it wasn’t going to.” Having established they would be within range of medical help if necessary, she cleared them to go. However, their car hit a bad pothole on the way, resulting in a blowout of two tyres, and they never got there.
“It was literally a blessing in disguise because by the time we got back to the house we had been staying in, Alby had just got so much worse. He wasn’t able to keep any feeds down.”
On the Wednesday they used the nebuliser but his breathing was getting fast and raspy. The following day they rang the doctor again and she sent them to a physio, to work on moving the phlegm from his chest and using nasal suction to remove it.
“He got worse so fast, it was frightening,” says Sinéad. By the end of the appointment, the physio advised them to take him to the hospital emergency department.
“They had him on oxygen within 20 minutes of us arriving in A&E. His saturation levels were very low and he was really struggling to breathe.”
After Alby was discharged, they weren’t allowed to fly home to Dublin for another week, to give him a chance to regain his strength. But very soon, “he was like a new child, it just cleared up”.



