Epstein-Barr virus (EBV) is a member of the herpesvirus family that infects 95 per cent of the world’s population at some point in their lives. It causes infectious mononucleosis (IM), aka glandular fever, and it was the first human cancer virus to be discovered.
Two of the four main players involved in its discovery were born in Ireland, and three of them were educated here.

One evening the London-born pathologist Dr Michael Anthony Epstein, who is now 101 years old, attended a lecture he had seen advertised at the Middlesex Hospital Medical School, where he worked. The notice announced that on March 22nd, 1961, at 5.15pm, “Mr DP Burkitt from Makerere College, Uganda will talk on, ‘The Commonest Children’s Cancer in Tropical Africa: a hitherto unrecognised syndrome’.”
Denis Parsons Burkitt (1911–1993) was born at Lawnakilla, near Enniskillen, Co Fermanagh. He attended Portora Royal School, and in 1935 graduated in medicine from Trinity College Dublin (TCD). Despite losing his right eye after a childhood accident, Burkitt qualified as a surgeon. A religious man, he felt drawn to work in Africa, and in 1957 at Mulago Hospital in Uganda’s capital Kampala he began documenting jaw tumours among children — a disease later called Burkitt’s lymphoma (BL).

BL’s epidemiology suggested that an infectious agent might be responsible, and after Burkitt’s 1961 lecture, Epstein, then working on a cancer-causing virus of chickens, wondered if a human virus might be implicated in BL. Collaboration began, with BL biopsies being flown from Kampala to London, where Epstein deployed traditional culture methods to recover virus, all of which failed.
I suppose it should have been called BL1 (Burkitt’s lymphoma) but somehow it got christened EB1 — E for Epstein, B for Barr, my maiden name
Until Yvonne Margaret Barr arrived.
Yvonne Barr was born on March 11th, 1932 at 1 Pembroke, Carlow town, and when her bank manager father was posted north, she attended Banbridge Academy, Co Down (1942–1949), where she was head prefect. In 1953, Barr graduated from TCD with an honours degree in natural sciences, majoring in zoology. Between 1955 and 1962 she developed cell culture expertise while working on leprosy and canine distemper virus at London’s National Institute for Medical Research and the University of Toronto, respectively.
A research grant from the United States National Institute of Health enabled Epstein to employ two research assistants. First to arrive at the Middlesex Hospital’s Bland Sutton Institute of Pathology was Barr, in September 1963. Private papers kindly supplied by Barr’s family provide telling insights into the discovery of EBV. “By the time I arrived at the Middlesex,” explains Barr, “I had a lot of tissue culture experience ... to my surprise, I felt Epstein was throwing out the good cells. I applied my methods and every few days gave the cells a wash and new food ...” The BL biopsies from Uganda, notes Barr, “were immersed in a transit fluid surrounded by ice in a small thermos flask and had a habit of arriving either at the weekend or late at night”.
Writing in 2012 — Burkitt lymphoma and the discovery of Epstein-Barr virus — Prof Sir Michael A Epstein recalls that “on Friday, December 5th, 1963 a flight from Uganda was diverted to Manchester by fog and we were only able to retrieve the biopsy in the afternoon when the plane finally reached London ... the usual transit fluid was cloudy, suggesting bacterial contamination ... ” However, Epstein “was astonished to find the cloudiness was not due to bacteria but to huge numbers of viable, free-floating lymphoma cells shaken from the sample on the unusually long flight ... free-floating cells from this delayed sample were set up in suspension ... ”
Barr routinely observed the suspension cultures for a pH change or increase in turbidity, stating that “on the twenty-sixth day [December 31st, 1963] such a change was noted in one of the cultures and so it was divided in two. At this time, I noticed some bright, glistening free-floating cells. They were lymphoblasts – a cell type that little was known about. I called the boss [Epstein] in, but he could not see them. I will never forget – I said to him ‘rack the microscope down’ and he did; he went right through the glass. What a disaster! Once the air got in, they were contaminated and that was that.” Barr, however, had taken the wise precaution of splitting the original culture in two and the duplicate had viable cells too: “From this container,” writes Barr, “the first EB1 line was established”.
A vaccine could be some way off. One must remember that most people live healthy lives while the virus lies sequestered in the B cells of their bodies
Barr’s papers reveal an important observation: “I suppose it should have been called BL1 (Burkitt’s lymphoma) but somehow it got christened EB1 — E for Epstein, B for Barr, my maiden name.”
The second of Epstein’s research assistants Dr Bert Geoffrey Achong (1928–1996) was born in Port of Spain, Trinidad, and in 1953 graduated in medicine from University College Dublin (UCD). In 1971, and skilled in electron microscopy, Achong would later discover a “foamy virus”, the first example of a retrovirus naturally infecting man. But in late 1963 Achong joined Epstein and Barr and was given the option of using electron microscopy to study BL cells or liver cancer. As Prof Dorothy H Crawford and colleagues note, Achong decided on BL ... after tossing a coin.
It was time to use electron microscopy and search for viruses in the newly established EB1 cell line, and on February 24th, 1964 Epstein saw “a cell filled with herpesvirus”! Euphoric, he switched off the electron microscope and “walked round the block without a coat in the snow.” Rapid publication of their findings followed — Virus Particles in Cultured Lymphoblasts from Burkitt’s Lymphoma (Lancet) — and in 1965 UCD awarded Achong an MD for his work on the ultrastructure of BL cells.
As for the naming of the virus, Epstein remembers that the virus was sent to Dr Werner and Dr Gertrude Henle in Philadelphia for further study: “Subsequently, when the Henles came to publish further on it they began to refer to it as EBV after the EB cells in which we had sent it to them and that name was generally adopted.”
Meanwhile, Epstein encouraged Barr to use the project and undertake a PhD thesis, which was awarded in 1966 by the University of London to Yvonne Balding (in 1965 she had married an industrial chemist from Melbourne, Australia). In May, 1966, the Baldings emigrated to Australia, where they had two children. Yvonne became a secondary school teacher and taught science and mathematics in the Melbourne area from 1973 to 1993 before retiring.

What of EBV research today? Patrick Naughton is a medical scientist working in the haematology department of Cork’s Mercy University Hospital and undertaking a postgraduate research PhD at Munster Technological University on the investigation of IM with a view to developing a national standard procedure for its investigation. Naughton told The Irish Times: “There is a strong association of EBV with BL, Hodgkin lymphoma and certain B-cell lymphomas, and an association with epithelial cell cancers; in particular nasopharyngeal carcinoma and to a lesser degree gastric cancers.” More recently, says Naughton, several papers have emerged suggesting a link between EBV and multiple sclerosis, and there is also an association with various autoimmune diseases.
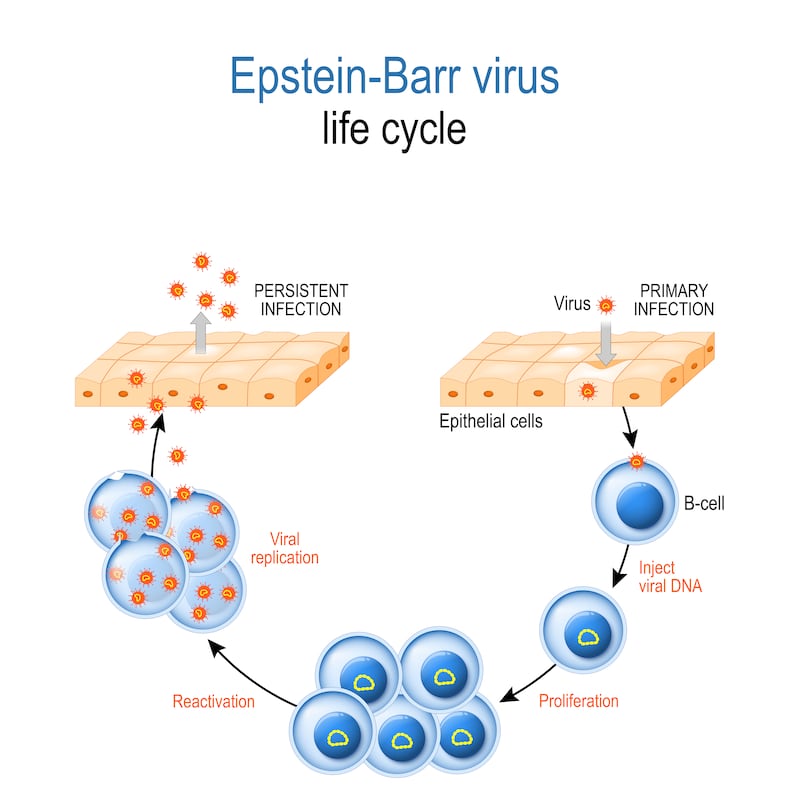
EBV, explains Naughton, has developed an elaborate means of hiding inside the B cells of the human host: “The body, following primary infection, is in a constant state of defence against the virus and in certain cases this can lead to the development of autoimmune diseases against the cells harbouring the infection. In most healthy individuals the parasite/ host balance is maintained without any great compromise to health but in cases of stress or lowered immunity the virus proliferates and overpowers the host and disease can manifest, this is particularly evident in cases of post-transplant lymphoproliferative disorders.”
Is an EBV vaccine possible? Extensive research, Naughton explains, is being undertaken, “but a vaccine could be some way off. One must remember that most people live healthy lives while the virus lies sequestered in the B cells of their bodies. Another area of research is the development of antiviral therapies, but this research is in its infancy and results have to date proven inconclusive.”
In Ireland, Naughton thinks that the development of a standard national procedure for the investigation and subsequent testing for IM, the primary disease caused by EBV, would benefit the Irish health service: “Correct and prompt diagnosis of IM can help prevent the unnecessary administration of antibiotics and mitigate the need for other expensive exploratory tests in the search for a diagnosis; a standard testing procedure would enable clear, unambiguous diagnosis of the disease, particularly in atypical cases, resulting in shorter hospital stays, and saving time and money.
Naughton emphasises the importance of a collaborative approach between clinician and scientist to benefit all concerned: “You only need to consider how such an approach between clinician Denis Burkitt and the laboratory scientists Epstein, Barr and Achong ultimately led to the discovery to the world’s first oncogenic virus and all that has followed. Knowledge,” says Naughton, “is the key, and shared knowledge and collaboration will get us to where we need to go a lot quicker than a singular approach.”











