
Despite affecting up to 10 per cent of women, endometriosis is not often talked about and not fully understood. It is surrounded by taboo, myths, poor or delayed diagnosis, and unreliable treatments. Regardless of how common the condition is, one in ten women living with this gynaecological issue may not have received a diagnosis for up to nine years as the symptoms imitate those of other conditions. This chronic condition arises when tissue, called the endometrium, grows in other places in the body. These growths may result in a chronic inflammatory reaction causing pain or scarring with an effect on infertility.
As with any condition that is misunderstood and complex, many people avoid seeking help for the condition despite it having a profound affect on a person’s life, physically, mentally, and socially.
To help debunk the misconceptions and myths of endometriosis, Iryna Ilyich, medical adviser at Flo Health, clarifies some of the intricate misunderstandings concerning the condition.
1) Myth - It is easy to diagnose endometriosis
On average in Ireland, it is reported to take nine years to diagnose endometriosis as the symptoms of the condition are similar to other disorders such as irritable bowel syndrome or pelvic inflammatory disease. As such, symptoms alone are not enough to diagnose endometriosis.
Safe Harbour review: Jack Gleeson and his moustache steal gangland drama from a menacing Colm Meaney
I think Putin is testing Trump, to see how far he can go and how many advantages he can get
Hey, tourists: fondling the Molly Malone statue is not a Dublin tradition. And it probably won’t bring you any luck
‘My partner broke up with me to ‘find himself’ – but still texts me every day’
“Various studies report a global diagnostic delay of seven to nine years when it comes to endometriosis,” says Ilyich. “This delay may lead to the deterioration of mental health and low quality of life due to chronic pain, higher healthcare costs, and worsened outcomes of infertility treatment.”
Recognising the impact endometriosis can have on a person’s life highlights the importance of receiving a diagnosis as early as possible; and the only definitive way to diagnose endometriosis is through surgery.
“In order to diagnose endometriosis, a doctor would need to perform a routine examination,” says Ilyich. “It all starts with a pelvic exam during which the doctor manually feels or palpates areas in the pelvis for abnormalities. Then, you would probably require a series of imaging tests such as an ultrasound, computed tomography (CT) scanning, or MRI (magnetic resonance imaging) to essentially get a visual of the inside of your body. A standard ultrasound test wouldn’t definitively tell the doctor if the patient has endometriosis, but it can identify cysts associated with it. For some, an MRI or a CT scan can help with surgical planning, giving the surgeon detailed information about the location and size of endometrial implants.”
In some cases, a laparoscopy is needed to determine the diagnosis of endometriosis. “This procedure allows the surgeon to see inside the abdomen,” explains Ilyich. “It’s performed under general anaesthesia, with the surgeon making a tiny incision near the navel and inserting a slender viewing instrument called a laparoscope to look for signs of endometrial tissue outside the uterus. Laparoscopy can provide information about the location, extent, and size of the endometrial implants. It also allows for a tissue sample, or a biopsy, to be collected for further testing.”
2) Myth - Women with endometriosis cannot have children
The most foreboding of myths concerning endometriosis is the belief that those with the condition cannot have children, yet it is believed that about half of women with endometriosis go on to have children.
“In general, pregnancy is possible for women with endometriosis, but it depends on the severity of the condition,” says Ilyich. “It’s important to note that endometriosis is considered to be one of the three major causes of female infertility. According to the American Society for Reproductive Medicine, endometriosis can be found in 24 per cent to 50 per cent of women who experience infertility. Up to 30 per cent to 50 per cent of women with endometriosis may experience infertility.”
The condition can influence fertility in several ways, advises Ilyich, including distorted anatomy of the pelvis, adhesions, scarred Fallopian tubes, inflammation of the pelvic structures, altered immune system functioning, changes in the hormonal environment of the eggs, impaired implantation of a pregnancy, and altered egg quality.
“Studies show that the chances of becoming pregnant can be improved with surgical treatment,” explains Ilyich, especially if endometriosis is in the moderate to severe range. “The combination of surgical and medical therapy may be beneficial in patients attempting to conceive through in vitro fertilisation (IVF). Overall, treatment is highly individualised for each patient.”
3) Myth - Endometriosis improves after menopause
“For some women, the painful symptoms of endometriosis improve after menopause,” says Ilyich. “As the body stops making the hormone oestrogen, the growths shrink slowly. However, some women who take menopausal hormone therapy may still have symptoms of endometriosis.”
In addition, hormonal treatments such as the pill, while they may suppress symptoms, do not have a long-term effect on the condition, with symptoms likely to return once treatments stop. Furthermore, a hysterectomy may relieve symptoms, but the condition can reoccur with persistent symptoms despite the surgery. Nevertheless, it is important to understand that the symptoms of endometriosis can be reduced with the right treatments and management plan.
4) Myth - Endometriosis is always painful and just like a heavy period
The assumption that a painful period or a heavy flow is a normal occurrence of menstruation can have a damaging effect on those with endometriosis who subsequently fail to report their symptoms to their doctor. An additional concern a person has is the fear of being dismissed by the medical profession for overreacting or exaggerating their symptoms. And yet, not everyone experiencing endometriosis suffers pain with a diagnosis of endometriosis coming to light once fertility issues are investigated.
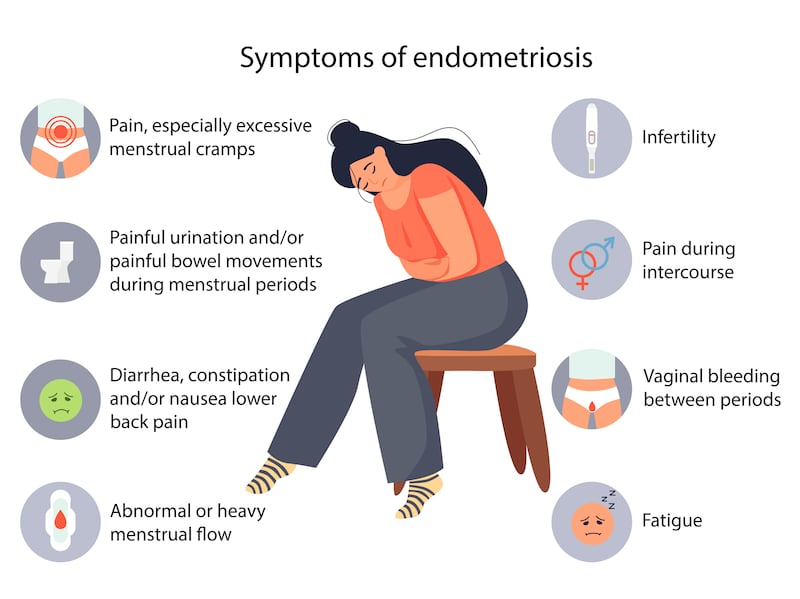
“About one-third of women with endometriosis remain asymptomatic,” says Ilyich. “Symptoms of endometriosis can vary but they typically reflect the area of impact. Such symptoms may include dysmenorrhoea (painful periods), heavy or irregular bleeding, pelvic pain, lower abdominal or back pain, dyspareunia (painful sex), dyschezia (pain on defecation) often with cycles of diarrhoea and constipation, bloating, nausea, and vomiting, perineal pain, pain during urination, blood in the urine, and pain during exercise.”
5) Myth - Endometriosis can be prevented
“No one knows for sure what causes this condition,” suggests Ilyich. “That is why we don’t know how to prevent it. While any woman can develop endometriosis, the following groups seem to be at a higher risk: those with a family history of endometriosis, delayed childbirth (women aged 30+ giving birth for the first time), starting period at an early age (people who begin menstruating before the age of 11 may be at a higher risk), short menstrual cycles averaging less than 27 days, long duration of menstrual flow, heavy bleeding during menses, any medical condition that prevents the passage of blood from the body during menstrual periods, or low body mass index.”
While there is no cure, there are several treatment and management options, all of which are dependent on the individual and their unique situation.
For more information, visit The Endometriosis Association of Ireland - www.endometriosis.ie












