The homeless population is among the most marginalised section of our society – one that is over-burdened with complex and chronic physical and mental health difficulties.
Despite a population with great medical needs, the homeless are also among the least served when it comes to accessing the mainstream health service.
Epilepsy is one of a number of physical conditions that is over-represented among the homeless population and an innovative project run between the Epilepsy Service and the Inclusion Health Department in St James’s Hospital in Dublin, together with the medical charity Safetynet Primary Care, is bringing epilepsy care directly to homeless people in the community.
The project was one of 122 projects across the country to receive funding from the €20 million Sláintecare Integration Fund.
According to Epilepsy Ireland, "epilepsy is a neurological disorder which affects the brain. It is a tendency to have repeated seizures".
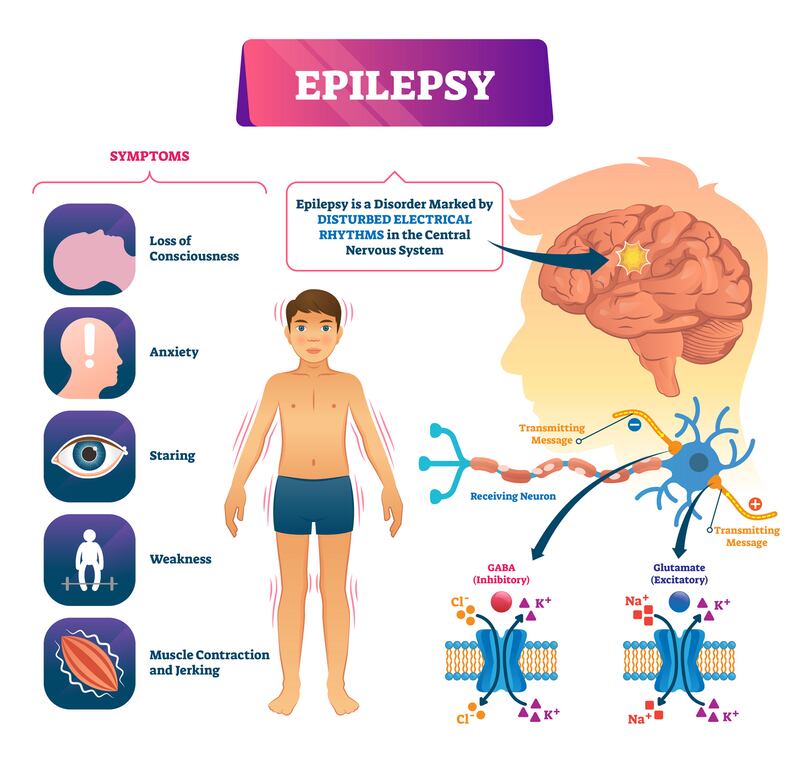
An estimated 40,000 people in Ireland have epilepsy and the condition affects 50 million people worldwide. It is the most common neurological disease of young people and one of the most common medical reasons for admission through the emergency department (ED).
Seizure disorder
The prevalence of epilepsy is eight times higher among the homeless population compared to the general population.
The new homeless outreach epilepsy project, which is run by consultant neurologist Dr Colin Doherty, together with Cara Synnott, Advanced Nurse Practitioner, Dr Elizabeth Doran, Specialist Registrar and Dr Cliona Ni Cheallaigh Consultant in Inclusion Health at St James's Hospital, in partnership with Safetynet GP Dr Enda Barron, aims to reduce ED visits by the homeless by 30 per cent and improve overall care for this group by providing an outreach epilepsy service in the community.
The project also aims to work with GPs who care for those with an intellectual disability and epilepsy to extend the outreach service to this population as well.
Cara Synnott, advanced nurse practitioner in adult epilepsy in St James’s and the Dublin Mid-Leinster Epilepsy Service, is one of the leads in the new outreach epilepsy programme and said her suspicion was that for some patients, epilepsy may have been in part responsible for their homelessness.
“Frequently the people we meet are people who have a history of seizure disorder going back to their childhood so, there is certainly a concern that these people are homeless with something to do with their epilepsy condition but that is really hard to quantify.”
Cara also explained that people living in homelessness with a diagnosis of epilepsy could find it more difficult to leave homelessness due to the regular seizures that come with their condition.
“There are psychosocial aspects of living in homelessness that would make epilepsy worse and even people who are living with epilepsy who don’t have that lifestyle, if they are going through times in their lives where it is chaotic where they are not sleeping well or using alcohol and drugs, well then their epilepsy will get worse,” she said.
The epilepsy service at St James’s Hospital has developed an effective and important integrated care pathway for seizure presentations to the ED.
In 2013 in St James’s, epilepsy was responsible for more than 1,000 ED attendances and 436 admissions with an average length of stay of five days. This figure has dropped to less than half that today with the use of an integrated pathway designed by the epilepsy team in the hospital.
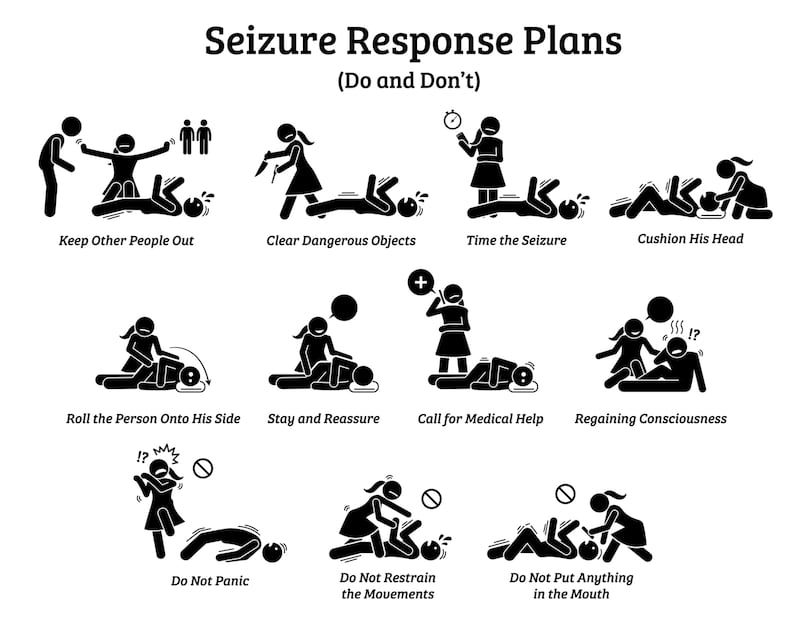
Under the integrated care pathway, when people present to the ED in St James’s Hospital with a seizure and are well enough to be discharged following necessary tests and investigations, they are discharged home and receive a fellow-up call within 10 days and a review in the epilepsy clinic within four weeks.
However, due to the chaotic nature of their lives, it is difficult for the homeless population to attend the clinic and be available for or even have a fixed address to receive details for their appointment.
Diagnosis
Dr Enda Barron, GP clinical lead with Safetynet, explained that a number of homeless people with a diagnosis of epilepsy were presenting to the service either after having seizures or were off their medication, and it was difficult to link them back into the specialist services.
The new project at St James’s uses a number of methods including, virtual outreach, a homeless epilepsy clinic and intelligent e-support for Safetynet GPs to help them deliver the same successful integrated care pathway developed by St James’s to homeless people with epilepsy in the community.
The project includes a pro forma questionnaire designed by the epilepsy service in St James’s. So, when a homeless person with epilepsy presents to Safetynet, the GP fills out the questionnaire and submits it via email to the specialists in St James’s, who review the details and send back an integrated care plan that the Safetynet GP can implement with the patient in the community.
The care plan might include a change to medication or a need for further investigations like an MRI or EEG. The Safetynet team includes nurses and key workers who can support an individual to attend an outreach clinic or hospital appointment if required.
Statistics have shown that 78 per cent of people with epilepsy who die from a seizure did not have any epileptic medication in their system and adherence to medicines can be a particular challenge for the homeless population.
In an effort to address this, Safetynet GPs work with staff in homeless hostels to ensure they remind clients to take their medication and if a patient is attending a methadone service they can receive their anti-epileptic medication at the same time as their methadone.
The outreach programme also includes a facility that allows Safetynet GPs to take blood samples to be sent to St James’s to test for levels of anti-epileptic drugs, which helps with the medical management of the condition.
“With this access to the blood service . . . we know if someone has been taking their mediation and if they haven’t, we know we don’t have to change the dose of medication we need to change the supports that need to be put in place to support the person in taking the medication,” Dr Barron explained.
According to Dr Barron, “often it’s about being able to respond effectively and efficiently as they present in front of you on that day. So this service has been a year in place with James’s and it is working really well. What a lot of the doctors in the community would find is that getting access to that specialist advice is the key to be able to provide a better point of care when patients present and this facilitates that. It is an amazing service to have access to those specialists services under this protocol.”
Sláintecare
Dr Barron said that the epilepsy project developed by St James’s was a model that could be replicated to treat other chronic conditions that are equally highly prevalent among the homeless such as diabetes or respiratory illnesses.
Dr Cliona Ni Cheallaigh, Ireland’s first ever consultant in inclusion health and associate professor in the department of clinical medicine in TCD, agrees that the epilepsy project is one that can be replicated for other chronic conditions.
Dr Ni Cheallaigh also received funding under the Sláintecare fund for two additional nurses to provide a similar outreach programme in diabetes, chronic obstructive pulmonary disease, other neurological conditions and chronic venous ulcers.
“So we are trying to take the epilepsy model and use it. It works perfectly for other chronic conditions and we have loads of really good consultants and specialist nurses in James’s who are keen to reach out to this population,” she said.
Commenting on the importance of outreach services for the homeless and bringing care to where it is most needed, Dr Ni Cheallaigh said that the homeless population were those with the highest need but also those that find it hardest to attend hospital or for whom the hospital setting is not designed and it is also a place where the homeless are most poorly represented.
“How many CEOs and consultants and nurse specialists are from a Traveller background for example, or have lived experience of homelessness or opiate addiction? Very, very few. So when we are designing our services . . . they don’t feel it’s their place and we don’t necessarily make them feel it’s their place,” she said.



















