Since the start of 2021, seven Irish citizens have died after seeking medical, cosmetic or dental treatment in Turkey.
Two people died in 2021 and four in 2022, according to the Department of Foreign Affairs (DFA), which is aware of the case of a seventh person, a man, who died in Turkey during a dental procedure just last month.
Separately, it is understood that another Irish person, a woman, who travelled to Turkey for a dental procedure has also recently died, but the precise cause of death remains unknown.
Sources in the Health Service Executive (HSE) are concerned that the actual number of deaths is probably higher, since not every death abroad has to be reported to the DFA.
Sally Rooney: ‘I enjoy writing about men ... the dangerous charisma of the oppressor class’
Alzheimer’s: ‘I’ve lost my friend and my companion,’ says Úna Crawford O’Brien of fellow Fair City actor Bryan Murray
Ryan Adams at Vicar Street: A gig that nobody will forget anytime soon, but perhaps not for all the right reasons
The phenomenon of travelling abroad for treatment is sometimes referred to as medical tourism.
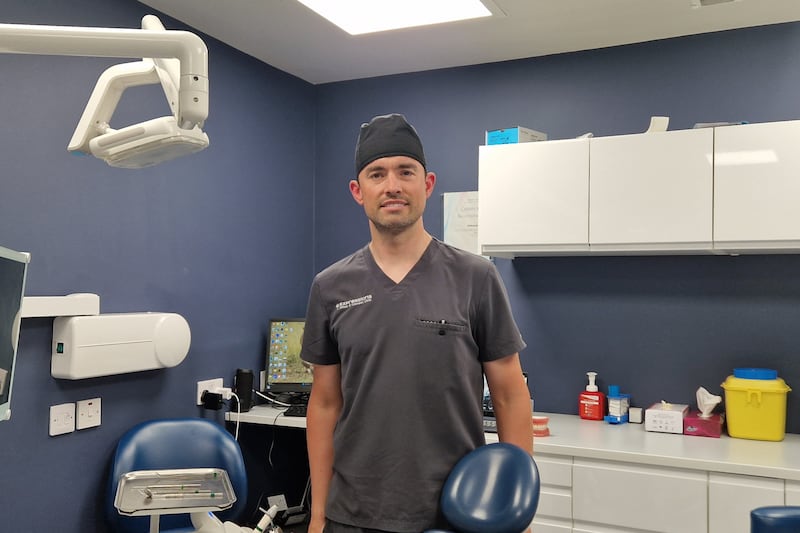
Dr Will Rymer, chair of the National GP Committee at the Irish Dental Association, is a practising dentist in Roscrea, Co Tipperary. He reports treating on average two patients a month presenting with complications having travelled abroad for dental work.
“The Irish Dental Association carried out a survey in 2018 where 74 per cent of Irish dentists reported having to deal with problems post-dental tourism,” Dr Rymer says. “They wouldn’t be as significant as the most recent case [of the man who died last month].
“Generally what’s happening is you’re having patients presenting to us having had extremely aggressive dentistry done. I might see a patient for a routine treatment, I might recommend to have a small filling, maybe a cleaning and if they’re interested in cosmetics you might offer a bit of tooth-whitening. At their six-month review, they come back having been away and they’ve had a block of porcelain crowns fitted across all of their teeth, they’re all fused together, they’re poor quality.
“Because two teeth are fused together, the entire smile is now dependent on every tooth being healthy. So if they get a problem with one tooth, we have to dismantle the entire smile. You go from a case where their mouth was a six out of 10, they’d have liked to go to an eight out of 10 but in reality they ended up with a one out of 10, they just didn’t realise it for a couple of years.
“I had a young chap, in his 30s, he had quite aggressive gum disease for a very young person. Apparently he had gone to see a friend in Turkey and his friend fit him with full porcelain crowns, his teeth were all fused together, which massively accelerated his gum problem.
“Over the course of two years we’ve dismantled it to the point we’ve fitted him with full dentures. It’s a huge deterioration in his oral health, something that could have been avoided with intensive, specialist gum care.”
According to Dr Rymer, in the past the primary motivation behind dental tourism was the lower cost in countries such as Turkey. However, he says that a range of other factors are now at play, leading to an increase in people presenting to him with complications since the end of the Covid pandemic.
[Dental tourism is caused by] a perfect storm of the cumulative effect of Government neglect of the medical card and PRSI schemes, lacking dentists, the lack of actual appointment time available and the economic situation, the perception of cheap dentistry elsewhere
— Dr Will Rymer
“Access is now a problem,” he says. “A lot of the patients previously would have been medical card patients who cannot get appointments because that scheme is in collapse. They’re now looking at Irish private prices and that’s a big jump from when they were getting treatment free of charge. There’s an economic impact but also an access problem. The medical card, the PRSI scheme, they’ve all suffered years of neglect, those people are now having to employ increasingly desperate tactics to get seen.
“We have a huge problem with the number of dentists working in Ireland, we actually have a significant shortfall. It’s a perfect storm of the cumulative effect of Government neglect of the schemes, lacking dentists, the lack of actual appointment time available and the economic situation, the perception of cheap dentistry elsewhere.”
Dr Rymer says some commercial entities are “preying” on these access and cost issues to exploit Irish patients. “I know a lot of very good Turkish dentists,” he says. But they are not part of what he described as some of “the commercial enterprises that are touting for patients in Ireland and preying on the fact that these patients are vulnerable”.
“If they’re not in mainstream media, those ads are all over social media. As soon as you have searched for cheap ways of getting your teeth fixed, various search engines are going to feed you ads that get you what you want.
[ Dentists pass vote of no confidence in Minister for HealthOpens in new window ]
“What happens is that a clinic will pop up, treat a bunch of patients and then disappear. There’s no comeback for indemnity or insurance issues, the clinic has vanished, the owner has vanished, the dentist has vanished. There’s very little opportunity for the patient to have the problem remedied.
“Now they’re facing a much bigger bill to try to put things back and get reasonable health again.”
A Department of Health spokesman said that the Government invests over €200 million annually into the provision of oral care in Ireland, targeting “those most in need of State support to access care.”
The spokesman said that the Government recognises that “substantive reform” of oral healthcare is required, while pointing out that there are more dentists working in Ireland than ever before.
According to the Department, €5 million has been provided in this year’s budget to support the HSE to assist patients to access emergency dental treatment through private contractors and HSE-employed dentists.
Away from dentistry, the most common treatments for which Irish people travel include weight-loss procedures, hair transplants and orthopaedic procedures such as hip and knee replacements. In the case of the latter, Prof Deborah McNamara, consultant surgeon at Beaumont Hospital in Dublin, warns of the danger of air travel after recent surgery. Particularly with lower limb procedures, sitting still in a confined space for an extended period of time increases the risk of blood clots.
“I know that orthopaedic surgeons are very concerned about people travelling abroad for bone and joint operations because of the very high risk of clots that those operations carry,” she says. “There is the increased risk that air travel brings and also the devastating impact if you have an orthopaedic implant put in place and you get an infection in that implant. That has life-altering side effects that are often permanent.”

Prof McNamara is also vice-president of the Royal College of Surgeons Ireland (RCSI). The college does not provide medical care, but Prof McNamara says engagement with surgeons involved in the organisation led to the publication last December of guidelines aimed at informing people thinking of travelling abroad for medical care.
“The reason we became interested is because we were hearing from surgeons around the country that they noticed an increase in the number of people returning from abroad having undergone surgery and experiencing complications who were presenting to hospitals through the emergency department,” she says. “In my own experience in Beaumont, we were admitting patients a couple of times a month who had been abroad for various types of surgery.
For a lot of surgery, infection is the significant risk of an operation ... There are some specific aspects, like travelling abroad, that increase that risk
— Prof Deborah McNamara
“Surgery always carries risk. For a lot of surgery, infection is the significant risk of an operation; that’s irrespective of where the operation happens. There are some specific aspects, like travelling abroad, that increase the risk of infection. We know that there is a different incidence of the so-called superbugs in other countries, the patterns of antibiotics used are different and we know the types of antibiotics vary from country to country.
“If you have an operation in Ireland you know it’s being supervised by a consultant surgeon who’s on the specialist list through the Irish Medical Council. You know that person has to take part in continuing professional development and report on that every year. You know they’re required to have indemnity if things go wrong. Those safeguards can’t be assumed to be in place in every country.”
In Britain, a recent study carried out by the National Health Service (NHS) found that, since 2019, at least seven British patients had died in Turkey having undergone weight-loss surgeries. Prof McNamara says that many people underestimate what such surgeries entail, particularly after the procedures. “Obviously the purpose of the operation is to lose significant amounts of weight and that has an impact on the body generally,” she says.
“There’s more to undergoing that procedure than just having the technical part of the procedure. The aftercare and follow-up is really important. Educating people in advance, having them understand the risks of surgery, helping them to have realistic expectations of what can be achieved, all of those are important factors.”
The majority of procedures sought by so-called medical tourists are cosmetic, as opposed to strictly necessary medical treatments. According to Prof McNamara, the risks of such “superficial” surgeries are not always explained to patients as extensively as they ought to be.
“I’m not sure everyone appreciates the risk that they’re taking, particularly in the area of cosmetic surgery,” says Prof McNamara. “It’s incredibly easy to register to have an operation or attend one of these clinics. I think that in some situations the operations are painted more as a lifestyle choice, more in the realm of cosmetic procedures that aren’t operations, that there’s a big difference between having an operation and going for other types of superficial cosmetic procedures that people might have.
“I think it might not be clear to people actually the degree of risk that they’re taking. One of the big factors is that surgery always carries risk for patients.
“The assessment and consultation ahead of theses procedures is really lacking in many cases that you hear about. I’m concerned that sometimes patients aren’t getting that advice preoperatively in the way that they should, in the way that we would consider normal professional standards.
“If they’re not getting that information then I don’t think that it’s fair to say that it’s self-evident that it’s risky, I’m not sure the average person thinks about that very much.
“Sometimes when people think they’ve done their research all they’ve done is look at the website associated with the provider of the procedure or the clinic, as opposed to looking for other sources of information. It’s about trying to share that information with the public generally.”

Juan José Manzano is a musician living in Dublin. In 2019, he travelled to Istanbul for a hair transplant. He says the cost of having the procedure would have increased tenfold if he had stayed in Dublin. “At that time here in Dublin, it was about €9,000- €10,000,” he says. “Not counting the flights – they sent a package which was the hotel, the transport from the airport, the clinic, the operation – I spent €1,200.”
Mr Manzano, describing himself as a “perfectionist”, says that he did ample research into the safety of the procedure and the reputation of the clinic before travelling. “I reassured myself that I was going to be okay, the clinic was one of the best clinics in Istanbul with the best reviews,” he explains. “I spent months researching different clinics, websites, different people’s reviews. All of my research brought me to two clinics that I liked the most and I chose one.
“I treated this as a real medical procedure. What I found out doing my research was that there are good clinics and bad clinics, legal clinics and illegal clinics. You can do a hair transplant in Istanbul for €500, but I went to a good place.

“At the end of the day I was going to country that is not my country. I don’t know the quality of the medical access and all those types of things. There is a big question here. The low-quality clinics are the ones that spend more money creating really attractive advertisements on Instagram and social media. Some of the good clinics don’t have social media. They have a proper professional website, full stop.”
Four years later, Mr Manzano says his hair “doesn’t look like how it was when I was 20,” but that he is delighted with the results and with his decision to travel. He also says that he was satisfied with the level of aftercare provided by the clinic. “The operation is one day, then you have to come back the next day, they clean your hair and explain everything.
“I stayed in Istanbul for eight days. You go down the street in the city centre and see lots of people with bandages on your head – you see a lot of people like yourself.”
The Turkish embassy in Dublin did not respond to requests for comment. A comment was sought from the HSE.






















